- +91-9171082108
- +91-9171083108
- admin@sathamanamclinics.com
- Hyderabad, India
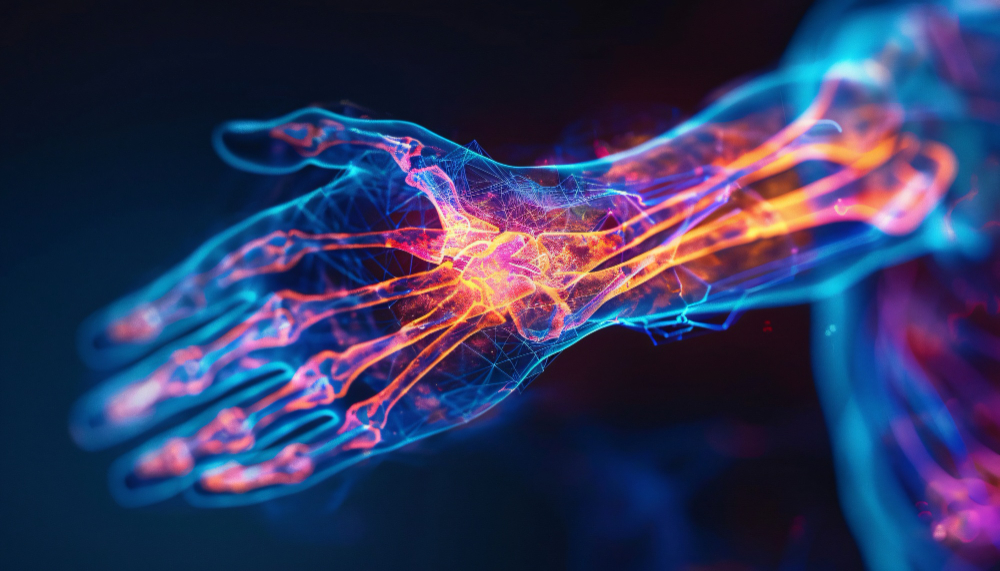
Diabetic Neuropathy: Understanding, Symptoms, and Management
Diabetic neuropathy is a common complication of diabetes, characterized by nerve damage resulting from prolonged high blood sugar levels. It can affect various parts of the body and lead to significant health issues, including pain, tingling, and loss of sensation. Understanding the types, symptoms, risk factors, and management strategies associated with diabetic neuropathy is critical for individuals with diabetes.
Understanding Diabetic Neuropathy
Diabetic neuropathy occurs when high blood glucose levels damage the nerves, leading to a range of neurological problems. Diabetes can affect different types of nerves, including sensory, motor, and autonomic nerves, leading to varying symptoms depending on the nerves involved.
Types of Diabetic Neuropathy
Peripheral Neuropathy: This is the most common form, affecting the nerves in the feet, legs, hands, and arms. Symptoms may include numbness, tingling, pain, and sensitivity.
Autonomic Neuropathy: This type affects the nerves that control involuntary bodily functions, including heart rate, blood pressure, digestion, and bladder control. Symptoms may include gastrointestinal issues, abnormal heart rate, and difficulty regulating body temperature.
Focal Neuropathy: Focal neuropathy affects specific nerves, often leading to sudden weakness or pain in one area of the body. This can include eye problems, Bell’s palsy, or nerve compression syndromes.
Proximal Neuropathy: Also known as diabetic amyotrophy, it primarily affects the thighs, hips, or buttocks, leading to pain and weakness in the legs.
Symptoms of Diabetic Neuropathy
Symptoms can vary widely based on the type of neuropathy, but they may include:
Risk Factors
Several risk factors contribute to the development of diabetic neuropathy, including:
Diagnosis
Diagnosing diabetic neuropathy typically involves:
Management and Treatment
While there is no cure for diabetic neuropathy, several management approaches can help alleviate symptoms and improve quality of life:
1. Blood Sugar Control
2. Pain Management
3. Lifestyle Modifications
4. Regular Check-ups
Conclusion
Diabetic neuropathy is a significant complication of diabetes that can lead to debilitating symptoms and affect quality of life. Early detection, effective blood sugar control, and personalized management strategies can help reduce symptoms and prevent further nerve damage.
If you suspect you have diabetic neuropathy or are experiencing symptoms, it is essential to consult a healthcare professional for proper evaluation and guidance. Contact Sathamanam Clinics for individualized care and support in managing your diabetes and related conditions. Your health is our priority, and we are here to help you navigate your journey to better well-being.
Empowering your health journey with personalized care, advanced treatments, and compassionate support at Sathamanam Clinics. Your well-being is our priority!